OVERVIEW
OVERVIEW
Coding integrity audits today generally share one characteristic in common: the reviewed claims make up only a small percentage of those billed. But, if you are only reviewing a portion of your billed claims, what “golden needles” might you be missing in the haystack of claims?
 CHALLENGES
CHALLENGES
Health systems frequently rely on external vendors and/or limited internal staff to audit their claims on a post-bill basis. However, as it becomes standard practice to focus only on specific Diagnosis Related Groups (DRGs), they frequently miss critical “golden needle” cases. These cases are uncommon but highly significant claims that have a substantial financial impact and usually exhibit three similar characteristics:
- Unusual Cases for Coding Staff
- Clinical Documentation Improvement Opportunities
- Coding Education Opportunities
Auditing a small portion of claims causes revenue leakage through limited reimbursement and quality inaccuracies, increasing payment delays and denials, leading to less revenue and higher collection costs. Furthermore, this limited scope overlooks crucial conditions and procedures within the patient population, resulting in an inadequate feedback loop for coding professionals.
 SOLUTION
SOLUTION
Analyzing 100% of your claims before the bill is issued is the holy grail for catching and correcting revenue & coding integrity issues proactively. However, manually analyzing all cases demands a level of staffing and time commitment that is not feasible for providers.
Introducing eValuator™
eValuator addresses this challenge with automated workflows and robust reporting tools, analyzing 100% of inpatient, outpatient, and professional fee claims. It flags potential revenue and coding issues before billing, enhancing staff efficiency and optimizing financial outcomes by identifying high-impact claims and infrequent “golden needles” prone to coding errors.
 FINDING THE GOLDEN NEEDLES
FINDING THE GOLDEN NEEDLES
Identifying those rare “golden needle” claims, whether through internal audits or with external vendor assistance, is streamlined with eValuator. In a recent sample, eValuator flagged claims that resulted in DRG changes, adding significant incremental net revenue such as:
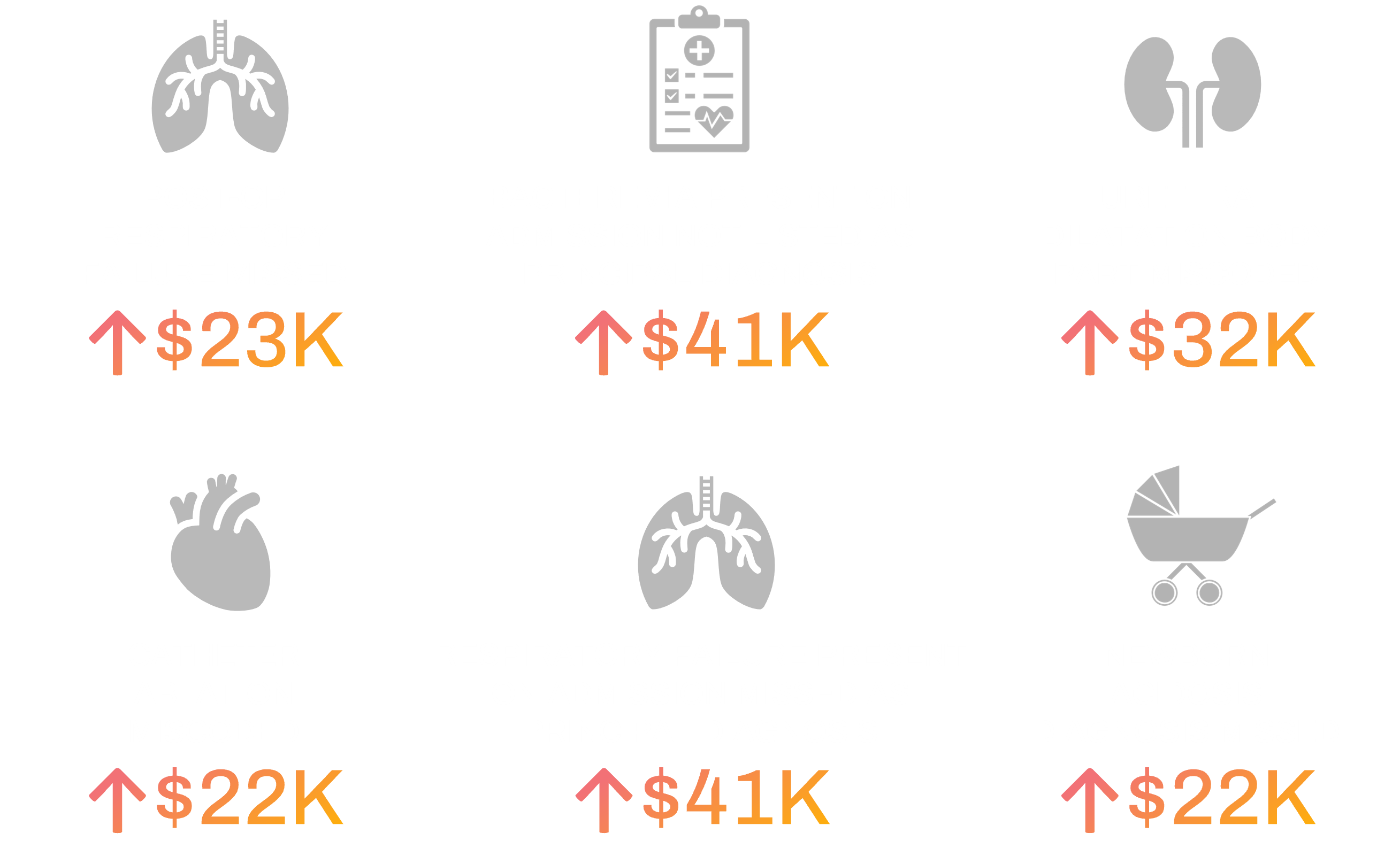
Identifying these “golden needles” also yields significant downstream benefits. One of our eValuator clients saved over $500,000 in contingency payments to their post-billing DRG validation vendor in their first year of utilizing eValuator for internal pre-bill reviews, achieved without additional staffing.
Another client noted that eValuator provides comprehensive insights into flagged claims, offering a complete narrative behind each review, including not only the financial impact but also the precise reason for flagging—an advantage absent in their previous technology, which only recommended an audit plan based on past quarter findings for already billed claims. This client also contrasted their former tool’s limited and generic algorithms, which prolonged the auditing process.